MS is a chronic autoimmune demyelinating disease of the central nervous system (CNS) and spinal cord. When the myelin sheath protecting the nerves becomes inflamed and subsequently damaged, signaling between axons is hampered and the otherwise protected nerve can decay. MS lesions are found throughout the CNS, including the cerebral cortex, and spinal cord; damage to these structures can cause severe, irreversible disability. Some of the most common presenting symptoms of MS include: optic neuritis (vision loss) transverse myelitis causing numbness and tingling and/or limb weakness, trigeminal neuralgia (facial pain), double vision and dizziness, and chronic fatigue. The diagnosis of MS requires a multi-modal approach to address the diverse pathology of the disease. It is often difficult and requires detection of abnormal lesions by brain and spine imaging.
MRI
Magnetic resonance imaging (MRI), is a crucial tool in diagnosing and monitoring MS. Traditional imaging techniques have not been sensitive to brain areas where lesions may develop. Originally, MS was thought to be a disease of the white matter, but in the last few years novel techniques have allowed lesion detection in the gray matter, which aids in diagnosis. These lesions have also been implicated in cognitive impairment., a common complication of MS.
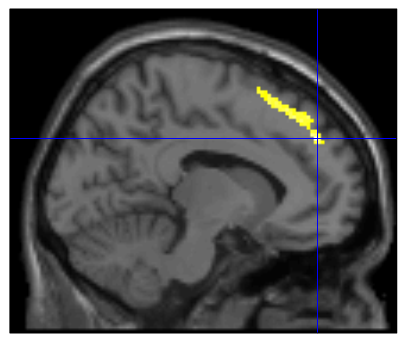
Unlike most clinical scanners in the country (1.5T and 3T strength), at the University of Minnesota’s Center for Magnetic Resonance Imaging (CMRR), we have ultra high field magnets (7 and 10.5 T) as well as novel imaging techniques to detect gray and white matter lesions in the brain of MS patients. Additionally, functional MRI (fMRI) has been proven effective at detecting changes in oxygen levels in the brain’s cortex. This level of oxygen saturation is referred to as BOLD (blood oxygen level dependent) activation and can be used to quantify damage to portions of the brain, based on how much oxygen the affected cells are using from motor, sensory or cognitive activity. fMRI allows detection of abnormal functions. Our research shows that cognitively intact MS patients have a significantly greater bold activation in relevant areas compared to those impaired.
At CMRR we are attempting to predict which MS patients are at high risk of developing cognitive impairment in order to determine the most efficacious window of time to introduce an intervention that could possibly hamper its development.
The enhanced capability of the 10.5T and 7T MRI units in detecting BOLD activation gives our research the greatest possible information in tracking the progress of MS and predicting how it will manifest in future.
Pharmacology
Early treatment with Disease Modifying Therapy (DMT) can both lessen the symptoms and slow the progression of MS. DMT’s are a number of commercially available medications in the form of pills, injections, or intravenous infusions. Traditionally, physicians prescribe these treatments as MS escalates over the course of a patient’s life. Research undertaken by our team seeks to ascertain if early treatment with higher efficacy (IV infusions) therapeutics can improve the life-long prognosis of those living with MS.
Improvements made to clinical practices surrounding how and why these drugs are prescribed could significantly improve patient outcomes and lay the ground-work for new pharmacological therapies More information on this research can be found on our Clinical Trials page, under ‘DELIVER-MS’
AHSCT (Autologous Hematopoietic Stem Cell Transplant)
The big question as it relates to MS is: ‘what if we could eliminate autoreactive lymphocytes and restart the immune system and eliminate inflammation?’ Essentially, can researchers break the cycle of inflammation that is causing nerve destruction in MS. AHSCT, or the transplantation of healthy, newly produced stem cells by the patient’s bone marrow, are collected before a chemotherapy session that eliminates the “defective” immune cells. The healthy stem cells are then re-infused and begin the process of rebuilding the immune system in a way that breaks the inflammation loop caused by MS. Currently, and generally, patients under fifty years old, who have had MS for ten years or fewer years and have had relapses or new MRI lesions despite treatment with other effective treatments, are considered the best candidates for AHSCT, this may offer some patients a state of complete remission.
Developments in the administration of chemotherapy are making this procedure safer all the time; a weakened immune system comes with inherent risks and discomfort, but could offer a real hope for remission. Though the results of treatment are so far encouraging, more research is needed to replicate the findings and to assess long-term outcomes.
Thus, improving the efficacy of stem cell transplantation is one of the key goals of the MSRC, and in combination with precise MRI and fMRI disease metrics, offers an exciting opportunity to for patients to take part in the BEAT-MS trial here at UMN: more information about the trial can be found on our Clinical Trials page.